It’s time for some serious talk. 1 in 5 of us would have suffered from a mental health disorder in the past year and over our lifetime that ‘1 in 5’ switches to 1 in 2. Scary right? But it’s time that we recognize the stats & start a conversation.
October marks Mental Health month, a chance for us to take a step back and think about our mental health, understand the importance of it, and encourage those around us to seek help if they need it. When it comes to tackling mental health disorders many of us often look to exercise, learning new skills, mindfulness, connecting with others, and medication to help manage things. And while there’s no doubt that each of these methods plays a key role in the management and treatment of mental health disorders, what if we told you that what goes into your diet could also affect your mental health?

GUT BRAIN CONNECTION
The gut-brain connection involves a two-way communication between the central nervous system (controls body and mind) and the enteric nervous system (controls the gastrointestinal system) linking emotion and cognition together with the gut. So, when we’re stressed out our brains can link emotional and cognitive areas of the brain with peripheral functioning of the gut potentially leading to abdominal pain or other gastrointestinal symptoms. On the other hand, when we have a poor diet and lack a diverse gut microbiota our gut can stimulate inflammatory responses to the brain which can affect mood and changes in behaviour.
It’s a lot more common than you think as well, let’s have a look at this example:
- When we’re feeling low and sluggish, we tend to reach for comfort foods high in refined sugar, fat and sodium which can be the answer to your prayers at the time but often lead to negative psychological effects such as anxiety and cognitive decline.
- On the other hand if we consume a wide variety of vegetables, fruits, wholegrains, legumes, nuts and seeds and oily fish we often see a reduction in mood swings, depression and anxiety, leaving us feeling more content.
RECIPE FOR HAPPINESS?
CARBS. CARBS. CARBS.Research suggests that eating high carbohydrate, low protein and low-fat foods can lead to a surge in the ‘feel-good hormone’, serotonin.
How? Well there is one theory that suggests that when carbohydrates release insulin, it triggers the entry of ‘tryptophan’ into the brain. Tryptophan is the key amino acid that forms of the building block of serotonin, so without it there would be no serotonin. Based on that you’d think that more tryptophan we have, then more serotonin we have & the happier we are, right? Unfortunately not.
Protein is the culprit in ruining that dream we’re afraid, as the minute you introduce too much protein into your diet the effects become redundant due to other competing amino acids trying to cross the blood brain barrier. In fact, you would have to boost the tryptophan through either supplementation or consuming pure starch to see the effects. Even potatoes, rice and flour contain too much protein. We know, bummer.
Contrary to this, other studies have repeatedly found positive effects with the more carbs consumed, the happier the subject. Moreover, studies that investigated low carb vs high carb diets often found improvements in mood, anxiety and depression in subjects following the high-carb diet1,2. However most trials are limited in duration and may only represent the short term advantages of a high carb diet which may be highlighting the avoidance of the ‘carb flu’
Although research is limited and quite complex, choosing complex carbohydrates, such those found in fruits, vegetables and wholegrains, will result in a more gradual release of insulin for potentially a more lasting effect on brain chemistry, energy and mood.
ANTIOXIDANTS
A diet high in antioxidants and anti-inflammatory foods such as fruits, vegetables and nuts can lower oxidative stress and inflammation protecting the brain from damage. Inflammation on the brain are also known to affect the neurotransmitters, dopamine and serotonin, which can contribute to decreased mental health. We recommend bumping up the berries, beans, dark chocolate (yasss!) and dark leafy greens.
PROBIOTICS & PREBIOTICS
Linking back to a healthy gut, diets high in prebiotic and probiotic foods and drinks may assist in colonising the gut to ensure a diverse gut flora which helps with proper hormone production for mood regulation. Do note that this area of study is relatively new so research often shows mixed results in the direct benefits with anxiety and depression. We say proceed with caution and opt for fermented foods (e.g. yoghurt, kimchi, sauerkraut) instead of formulated supplements. No matter the reasoning, a happy gut is always a good thing!
DEFICIENCIES
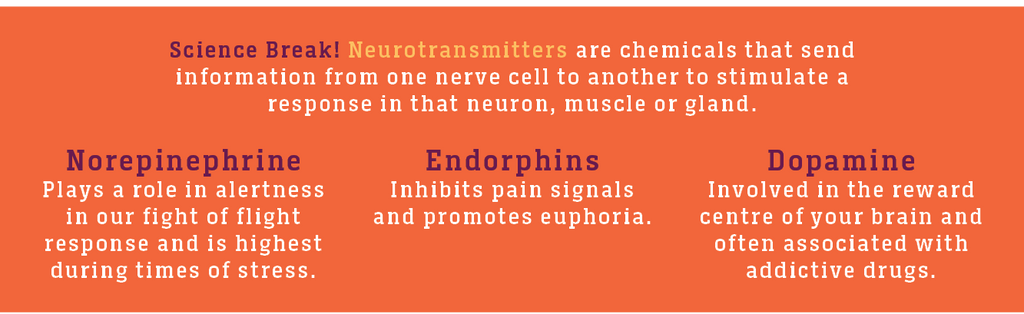
Reviews have indicated that a noticeable feature of patients suffering from mental health disorders were also deficient in essential vitamins (e.g. folate), minerals (e.g. magnesium) and omega-3 fatty acids3,4,5,6. A theory to explain this connection is that these nutrients are all precursors to neurotransmitters and those that are suffering from mental health conditions like depression are often deficient in neurotransmitters (serotonin, dopamine, noradrenaline and GABA).
OMEGA-3
Our brain is the fattiest organ in the body. Therefore, fats play a critical role on the brains ability to function and on our emotional and cognitive centres.
Researchers have long suspected the decline in consumption of omega-3 fatty acids as a factor in the increasing trend in higher incidences of major depression. This hypothesis stemmed from their ability to induce antidepressant effects when administered through daily supplementation. However, omega-3 fatty acid doses at 3g or higher did not exert a better effect and worked in opposition for those taking other medications.
Demographic data has shown that those that eat more fish had a lower incidence of mental disorders. Deficiencies in DHA (the other omega-3 fatty acid) have also led to lower serotonin, dopamine and norepinephrine all neurotransmitters in the good mood centre.
For an Omega-3 boost choose: Soy & Ginger Glazed Salmon with Vegetable Fried Rice, Salmon Risotto
FOLATE AND VITAMIN B12
Research published by the Journal of Biological Psychiatry indicated that patients provided with 0.8mg of folic acid a day or 0.4mg of vitamin B12 a day lead to decreased depressive symptoms. Clinical trials have also indicated that vitamin B12 were also shown to delay the onset of dementia although administration of this was strictly in a precise timing window.
Choose: Broccoli, Spinach and Kale Soup, Roasted Beef Fillet with Root Vegetables and Mushroom Sauce, Beef Lasagne.
MAGNESIUM
This same study also found that magnesium given at 125-300 mg with each meal and at bedtime also lead to recovery from major depression in less than 7 days for ‘most’ patients.
Choose: Soy & Ginger Salmon with Hokkien Noodles & Steamed Vegetables.
IRON
When you think iron, you think blood. What you might not know is that iron deficiency or anaemia during infancy are also linked to changes in cognitive functions and is also linked to apathy, depression and rapid fatigue caused in part by the a lack of transporting oxygen to the brain.
Choose: Korma Lamb Curry, Salmon Risotto, Chicken Burrito Mix.
Although this area of research linking nutrition and psychiatry is relatively new and for the most part based on observational studies, this field is growing.
The great thing is that nowadays mental health is better recognised, diagnosed, understood and treated, and if food can play a role in managing and treating mental health conditions, then it’s a step in the right direction. The things that we’ve mentioned above and the role they play in overall wellbeing are great to recognise, as it is another reminder of the benefits of a balanced diet that incorporates all of the food groups as recommended in the Australian Guide to Healthy Eating.
This month we challenge you to eat well, enjoy food with friends, and start a conversation about mental health.
To find out more head here for mental health month resources.